Here’s what’s worrying experts about bird flu right now — and what isn’t.


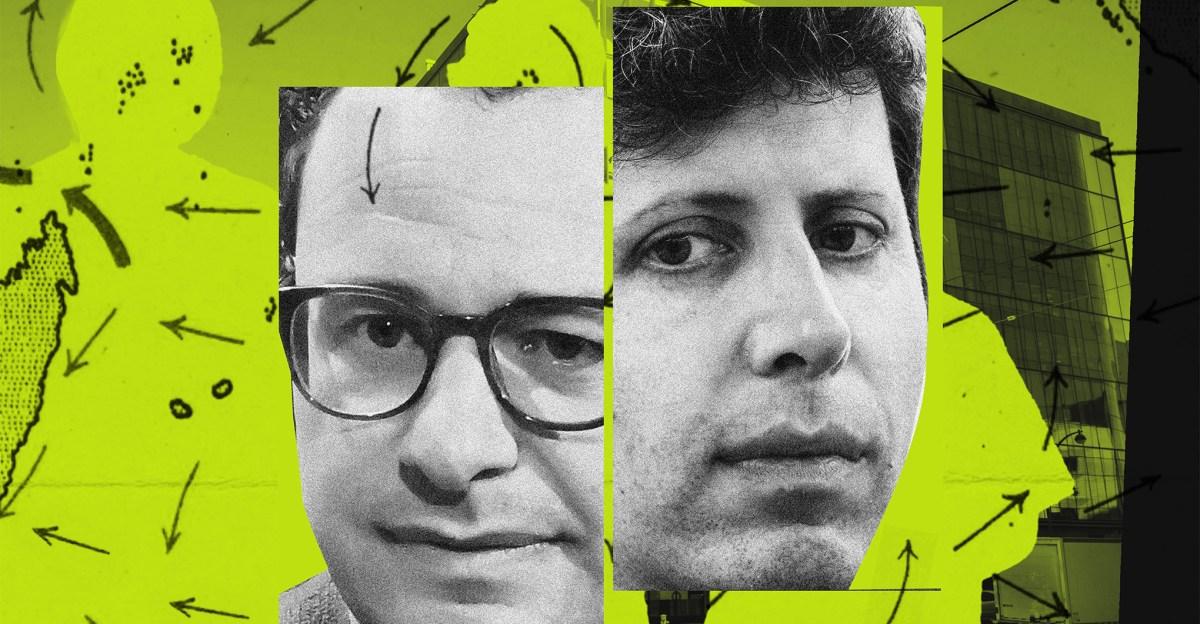
Last year, when an H5N1 avian flu virus — commonly known as bird flu — was spilling over from bird populations into a variety of wild mammals, Seema Lakdawala, a virologist and influenza A transmission specialist at Emory University, was “not overly concerned” about human risk. We don’t have “much of an interface with seals or with foxes, for that matter, or polar bears,” she says.
But when it comes to cows, that interface is vast. People on dairy farms regularly interact with cows and their milk; when the animals and their milk are infected with a virus that can cause disease in humans, and that mutates constantly, each of those interactions functions as an opportunity for the virus to workshop its adaptability. Now, says Lakdawala, “I am more concerned than I have been, and it’s not for the general public — it is for dairy workers.”
The H5N1 outbreak among cows on 34 dairy farms in nine states has so far led to only one very mild human infection. However, the virus was likely spreading among cows for months before it was detected. Lakdawala’s greatest concern is that this highly changeable virus has now arrived at an important point of human-animal convergence, and that we are not prepared.
For a virus to cause a human pandemic, it has to have three important characteristics, say flu experts. It has to cause human disease; it has to be something our immune systems haven’t encountered before; and it must spread easily among humans, especially through the air. The latest events do not yet demonstrate that H5N1 has new capacities in any of these categories. However, they hint that the virus has the machinery to evolve those capacities — and that it could do so before we know it.
In dairy cows, H5N1 has found an excellent laboratory for evolving traits dangerous to humans
Although Lakdawala was concerned when mink, seals, and other mammals were infected with H5N1 last year and the year before, cows are different. An outbreak among “mammals with a large interface with humans” is a red flag to her.
It’s a numbers game. Although all viruses mutate routinely, flu viruses are particularly good at shapeshifting and can even swap entire chunks of genetic material with other flu viruses if an animal is co-infected with more than one of them. These mutations happen randomly, and most don’t make the viruses more dangerous to humans — but it’s entirely realistic to imagine that some occasionally do. If that occasionally human-threatening mutation happens to a flu virus that has infected, say, a wild fox, it doesn’t pose a particularly high risk of causing a pandemic among humans. After all, few wild foxes have contact with humans. If it happens in a cow, however, there are far more opportunities for the virus to effectively workshop its new features.
People who work on dairy farms are constantly interacting with cows and their milk — they check udders, hook and unhook milking machines, and perform other tasks to care for the animals. That puts them in lots of contact with any virus infecting the cows. If the virus were one that didn’t infect and kill people or that doesn’t mutate and adapt as easily as the flu does, perhaps it wouldn’t be as concerning — but H5N1 does infect people at close proximity to animals, and at least half of the more than 900 people who’ve been infected with the virus since it came on the scene in 1996 have died.
“There is a high viral load in milk of these infected cows, and so it is a concern to me in terms of spillover [from] cows into workers,” says Lakdawala. “And the more often the virus has an attempt to spill over, the more likely it is to adapt.”
We already know the virus is adapting in mammals, she says. “The more spillover events, the more attempts that the virus has to find a successful variant that can take off or infect the human — and then one infected individual, three infected individuals, go home” to their families, where they could potentially spread the virus further.
It’s not a pandemic right now, she says, but now is the time to act to reduce the opportunities for spillover events.
For the first time, we have proof of H5N1 spreading among a mammalian species
When a virus leaps from one species into another, that’s not usually enough to cause a large outbreak. You could look at H5N1’s history: Although the virus has leapt from animals into people hundreds of times, it has very rarely spread among people. When infections effectively stop spreading once they cross species lines, the non-transmitting species is called a “dead-end host.”
Birds readily transmit H5N1 to other birds, but until recently, scientists have thought mammals getting infected with H5N1 were dead-end hosts. In the past couple of years, they’ve had some sneaking suspicion that minks and other mammals getting infected with the virus were spreading it among themselves — but they never had definitive proof. That is, they couldn’t rule out the possibility that all the animals had gotten infected by eating bits of the same sick bird, or through another so-called “common source” exposure.
It’s much harder to contain a pathogen’s spread within a species if members of that species can transmit it to each other. What the dairy cow outbreak shows for the first time is that mammals can indeed now infect each other with H5N1 — and can do it efficiently.
“Genetic data and epidemiologic data are all quite strongly suggesting that these viruses are getting transmitted in some way between these cows,” says Louise Moncla, a veterinary pathobiologist at the University of Pennsylvania School of Veterinary Medicine whose team has analyzed genetic data from infected cows that the US government recently made available.
This virus’s mode of transmission isn’t apparent yet — and it matters
It’s not yet clear how the virus is being spread through and between dairy cow herds. High viral loads in cows’ udders and in their unpasteurized milk make it possible that contact with contaminated milking machines is doing most of the transmission. However, it’s also possible the virus is spreading through the fecal-oral route or through contaminated air; the latter would be particularly concerning because it’s so much harder to prevent. (Moncla notes that while the classic genetic fingerprint for a bird flu’s ability to spread through air between mammals is absent from this strain of H5N1, that doesn’t mean we’ve ruled out respiratory spread.)
Regardless of exactly how H5N1 is spreading among cows, the significance that they’re transmitting the virus to each other is clear to flu experts: If the virus has adapted to spread among one mammalian species, it raises the specter that it can also adapt to spread among humans.
There is a precedent for flu viruses to spread from livestock to humans, leading to a pandemic: The 2009 H1N1 flu outbreak began when a flu virus spread from pigs to humans. It caused far less death than expected through a stroke of luck — because the virus had similarities to strains that circulated in the first few decades of the 20th century, many older adults still had some flu immunity left over from childhood infections.
If H5N1 develops the ability to spread among humans, it would be a novel infection to most immune systems, giving us much less protection from old flu infections. There are “no signs of that [ability] so far in the cattle sequences,” says Andrew Pekosz, a virologist who studies respiratory virus biology at Johns Hopkins University’s Bloomberg School of Public Health. “That’s a good thing.”
Still, because we don’t know much about how influenza A viruses like H5N1 behave in cows, we don’t yet know what cautionary measures will do the most to slow their spread. In 2011, scientists learned that the influenza D virus causes respiratory illness in cattle. However, not all flu viruses are created equal: “I did not ever anticipate seeing an influenza A in cattle,” says Lakdawala.
While influenza D infections don’t appear to cause much disease in humans, influenza A viruses very much do: All of the past global flu pandemics have been caused by influenza A viruses.
Because this is such an unusual event, says Moncla, “we know very little about how flu replicates and transmits in cows.” That makes it hard to quickly design and implement precautions to prevent the virus from spreading to the people who handle them.
“What would calm me down is if we started implementing interventions that would mitigate the presence of the virus and its transmission amongst cattle, and spilling over into humans,” says Lakdawala. “Say, okay: Every dairy farm worker is gonna wear a face shield,” she said.
It would help to know whether cows that are infected but asymptomatic have infectious virus in their milk, and whether they can transmit virus to each other, says Pekosz. Ongoing studies by academics and federal agencies should help answer those questions.
Here’s why you shouldn’t panic
At the moment, there are more “coulds” than “ares” with H5N1: Although the virus is showing that it could adapt further to spread among humans, so far it hasn’t; and while it’s reasonable to conduct studies to ensure pasteurization works against this particular strain of H5N1, there’s no reason to think it won’t.
It’s also worth noting that, according to a US Department of Agriculture representative who recently spoke to the press, the virus has so far not caused severe disease or death in the cows it has infected — they’ve all recovered with supportive care. In that way, this outbreak is very different from the ones we’ve seen in some other mammals.
Furthermore, testing at the Centers for Disease Control and Prevention has already demonstrated that existing antiviral medications are effective at preventing human infections with this strain of H5N1 and that two existing candidate vaccines could be used to rapidly scale up mass production of human vaccines against this virus if needed.
So for now, the general public shouldn’t be overly concerned about the virus, says Pekosz. “Scientists are … working extra overtime for this. But the general public should still feel safe.”

Google announces dates for I/O 2026
- 17 hours ago
PM Shehbaz calls for independent, sovereign state of Palestine
- 16 hours ago

Magnitude 5.6 quake jolts parts of KP
- 12 hours ago
Pakistan, US agree to enhance bilateral trade, economic ties, counterterrorism cooperation
- 15 hours ago

Scientists have found another alarming pattern in wildfires
- a day ago
Why it's so difficult to break into the Premier League's top six
- an hour ago

Strong earthquake rattles eastern Afghanistan
- 10 hours ago

Gold prices continue to surge in Pakistan, global markets
- 16 hours ago

It’s MAGA v Broligarch in the battle over prediction markets
- 2 hours ago
Money no longer matters to AI’s top talent
- 2 hours ago
PMD predicts dry weather in most parts of country
- 12 hours ago
NORAD detects Russian planes off of Alaska, sends aircraft in response
- 17 hours ago










