Bird flu has jumped from birds to cows — and now from cows to a human in Texas. Are we all at risk?


Bird flu is, famously, a disease that infects birds.
But on Monday, federal and state authorities reported that a person in Texas had tested positive for the disease, the second person in the US to contract avian influenza in the last two years. Stranger still, the patient didn’t contract the disease from a sick chicken or wild bird but from a cow, which was presumably infected with the virus. Rarely, if ever, have mammals infected humans with bird flu.
The Texas patient reported only one mild symptom — namely, pink eye — and is recovering, according to the Centers for Disease Control and Prevention. Yet the news is the latest in a long string of recent headlines that raise concerns about the risk that bird flu poses to public health. Avian influenza has ravaged domestic flocks, causing farmers to cull chickens by the millions. It’s also decimated wild birds and many marine mammals including seals and sea lions. And the virus is spreading, reaching penguins in Antarctica and at least one polar bear in the Arctic.
These developments are concerning. But how worried should we be? Here’s what to know about the risk to humans and to the millions of farmed and wild animals.
Bird flu basics: What it is, and where it comes from
Avian influenza, or bird flu, is a general term for the disease caused by influenza viruses that primarily infect and spread among poultry and some wild birds. They’re distinct from viruses that cause the flu in humans, though they’re related.
These avian viruses are quite common. They’ve been circulating for eons among wild waterfowl, such as ducks and geese, without causing them much harm. Mild forms of infection are called “low-pathogenic avian influenza,” or LPAI, which means they’re typically not deadly to wildlife.
The type of avian influenza spreading today is different. Occasionally, an LPAI virus can jump from wild birds to birds on poultry farms. As the virus replicates in densely packed warehouses of farmed birds, it can quickly evolve and adapt in ways that make it highly deadly to poultry. At that point, it gets dubbed a “highly pathogenic avian influenza virus,” or HPAI virus. That’s what’s circulating today — an HPAI virus.
Highly pathogenic bird flu has caused outbreaks on poultry farms many times in the past that have killed thousands to millions of farm birds. What makes this particular form of avian influenza virus so unusual is that it easily spreads and causes severe disease among wild birds and an increasing number of mammals. That’s rare.
The current strain of avian influenza spreading today descended from a virus that caused an outbreak on a goose farm in Guangdong, China, in 1996. The US first experienced one of these goose farm virus outbreaks in 2014 and 2015, which caused the death and culling of tens of millions of poultry birds and an unknown number of wild birds. Then in 2021, a related version of the virus arrived in the US — the cause of the current outbreak — that appears much better equipped at infecting wild animals.
Bird flu became big news in the months that followed, in 2022, when it started spreading through poultry farms. Farmers were forced to cull tens of millions of turkeys and egg-laying hens, often using a gruesome approach. It cost the federal government and the poultry industry hundreds of millions of dollars to manage and sent egg prices soaring in late 2022 and early this year.
Another person got sick. Does that up my risk?
The bird flu outbreak on poultry farms has, to an extent, dissipated, aside from a flare up in late 2023. Yet over the last two years, the virus has continued to spread — to different places and to different kinds of animals. Including mammals.
Early in 2023, the virus killed thousands of sea lions. In March 2024, officials confirmed that goats in Minnesota and dairy cows in Texas, Kansas, and Michigan also tested positive for bird flu. The USDA has also reported “presumptive positive test results” from dairy cow herds in New Mexico and Idaho. (The agency says milk, which must be pasteurized before entering the commercial food supply, remains safe to consume.)
“Although we don’t yet completely understand the factors that led to infection of the dairy cows with HPAI, it is possible that unique viral properties combined with epidemiological and environmental conditions all played a role for the spillover of HPAI into cattle,” said Diego Diel, an associate professor at Cornell University’s college of veterinary medicine.
What makes this concerning is the obvious fact that humans are mammals, too. As the virus makes the jump from birds to mammals, what’s stopping it from jumping to humans?
In the last few years, a couple dozen people worldwide — mostly in parts of Asia — have tested positive for this particular kind of bird flu, all of which likely came into close contact with infected animals. Symptoms may be nonexistent or subtle, such as eye redness or a mild flu, or they may show up as a fever (above 100 degrees Fahrenheit) and pneumonia and can prove fatal. In the last two decades, more than 800 people have been infected with bird flu globally, and more than half of them died.
In the US, however, human infections — let alone deaths — are rare.
The first human case of avian influenza from the current outbreak was in 2022, when a Colorado farmer who was involved in killing chickens tested positive. The man said he was tired for a few days but quickly recovered.
The person in Texas, meanwhile, tested positive earlier this year, after he was exposed to dairy cattle that were “presumed to be infected” with highly pathogenic bird flu, per the CDC. The patient is taking an antiviral medication and recovering, the agency said.
As for the rest of us?
First, the good news: The bird flu that infected the person in Texas (who is a dairy worker, per Politico) is almost certainly incapable of spreading dangerous infections to other people around the planet, experts say. Simply put, the virus currently does not have the proper biological machinery to easily invade — let alone circulate among — humans. We have very different physiologies than birds and other animals that HPAI easily infects. These workers got sick because they were likely exposed to very high levels of virus. (If you want to go deeper, check out our earlier explainer on this.)
TL;DR: The chances of you getting bird flu anytime soon are extremely slim.
The bad news is that influenza viruses evolve quickly, and unpredictably. Not only do they mutate, but they can also swap entire portions of their genomes with other viruses, creating new Franken-viruses, if two or more of them infect the same host. Under the right circumstances, this evolution could give the virus the tools to replicate more easily in mammals, which could make future strains of bird flu more threatening to humans.
Scientists are now racing to figure out what, exactly, those conditions might be. More specifically, they’re looking for signs that the virus is picking up adaptations that make it more likely to replicate within mammalian cells and — critically — to spread from mammal to mammal, such as cow to cow or seal to seal.
“There are many unanswered questions about the current HPAI outbreak in cattle, but one of the key questions is whether the virus is being transmitted from cow to cow,” Diel said.
One new study suggests that the virus has adapted to marine mammals and may be able to spread among them. USDA officials, meanwhile, have said that transmission of avian influenza among cattle “cannot be ruled out,” in a recent update about the dairy cow outbreaks.
“This virus is still relatively low risk for humans,” Marcela Uhart, a wildlife veterinarian with the University of California Davis School of Veterinary Medicine and senior author of the new study, said in a February statement. But she also had words of caution: “As long as the virus continues to replicate in mammals, it may make it a higher concern for humans. That’s why it’s so important to conduct surveillance and provide early warning.”
How should we be thinking about bird flu?
Obviously it’s not great that another human tested positive for bird flu. Again, he will likely be fine.
But this story is not yet over. Scientists are still trying to figure out how the virus is changing and what it means that cows are getting sick. The virus could evolve to become a risk, underscoring the importance of monitoring the outbreak closely.
There’s another tough reality here: Industrial animal agriculture, with thousands of animals packed together in warehouses, is a breeding ground for bird flu. So even if this current outbreak among birds wanes, we’ll likely continue to see new outbreaks in the decades to come, across different species. Eventually, that could pose a more serious risk to humans; the more chances bird flu gets to evolve, the more opportunities it has to turn into something dangerous.
That raises complex questions about our food system, and how we can make it healthier for humans — not to mention farmed animals and wildlife. To prevent or slow the spread of zoonotic diseases, like bird flu and Covid-19, governments, food companies, and farmers will need to invest heavily in surveillance (including of wild birds) and even vaccines, and they may ultimately need to make much more serious changes to animal agriculture.

Doctors temporarily recruited during Corona in Sindh fired
- 3 hours ago

Iranian hackers threaten to leak emails of Trump's close aides
- an hour ago

Pakistan's first int’l driving license kiosk set up at Lahore Airport
- 3 hours ago

Shadab Khan suffers shoulder injury, likely to rest for 3 months
- 26 minutes ago
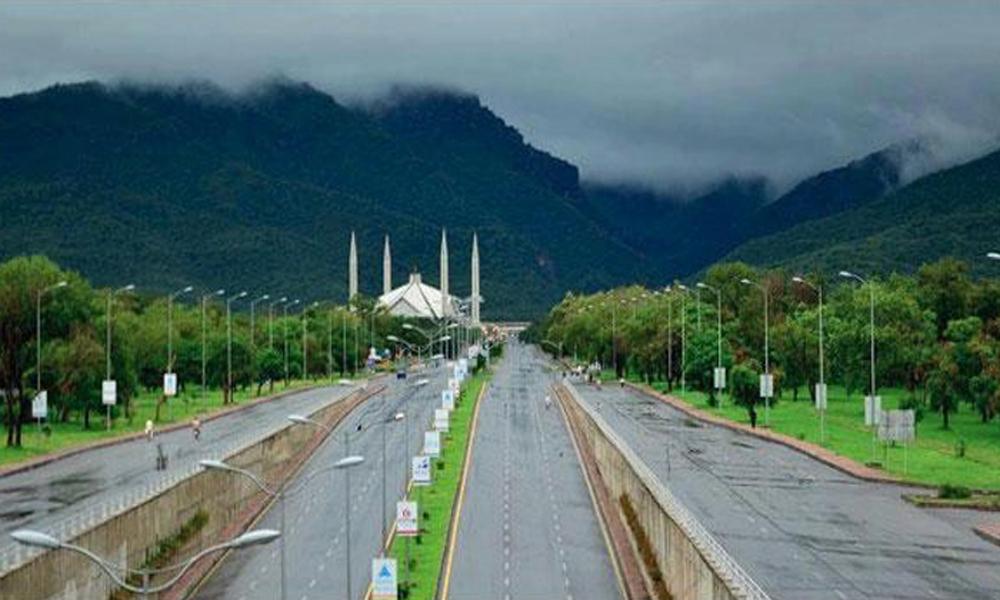
Torrential rain in Islamabad, Rawalpindi
- 5 hours ago

Govt surges prices of petroleum products
- 5 hours ago

Petrol, diesel prices increase in Emirates too
- 5 hours ago

Motorcyclist dies after being hit by water tanker in Karachi
- an hour ago

What we're hearing in the transfer window: Liverpool turn to Hato; Arsenal to make moves?
- 8 hours ago
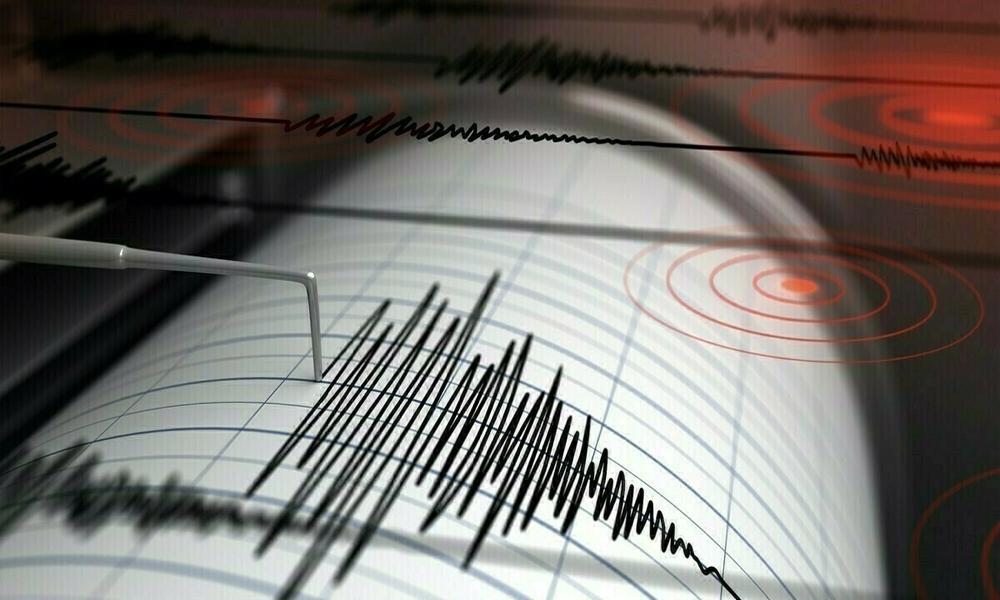
Strong earthquake tremors in Punjab including Lahore
- 2 hours ago

Thai court suspends PM over phone call leak
- an hour ago

Two terrorists killed in police, CTD joint operation in Bannu
- an hour ago









